Why are older adults more susceptible to dehydration?
- Muscle mass (an important store for water in the body) and kidney function tend to decline with age, thereby diminishing the ability to conserve water. This can make it more difficult to adapt to things like fluctuating temperatures.
- Your sense of thirst also diminishes with age. By the time someone actually feels thirsty, essential fluids could already be extremely low.
- Certain medical conditions and medications can affect ones ability to retain fluids. Dementia patients may forget to eat and drink and may experience difficulty swallowing (dysphagia) that prevents them from getting the fluids they need.
- Drugs like diuretics, antihistamines, laxatives and steroids can cause frequent urination that depletes water and electrolytes.
- Those suffering from incontinence may refuse or limit fluids in order to avoid accidents.

Symptoms of Dehydration in Elderly Individuals
Subtle signs of dehydration are important, as thirst is not usually a helpful indicator. A person who feels thirsty may already be dehydrated. Initial signs to look for include headache, constipation muscle cramps, dry mouth and tongue, and sleepiness or lethargy. Inadequate fluid intake is one of the most common causes of constipation.
Signs of Severe Dehydration
- Little or no urination
- Dark or amber-coloured urine
- Dry skin that stays folded when pinched
- Irritability, dizziness or confusion
- Low blood pressure
- Rapid breathing and heartbeat
- Weak pulse
- Cold hands and feet
Water helps to keep the urinary tract and kidneys healthy. When fluid intake is reduced the risk of urinary tract infections increases. Inadequate hydration is one of the main causes of acute kidney injury.
Everyone should aim to drink 1.5 litres (6-8 glasses) of fluid a day to stay hydrated
- All fluids other than alcohol contribute to fluid intake – alcohol has a dehydrating effect so doesn’t count
- Make sure they know how many glasses of water and other drinks your loved one is drinking and offer a choice to avoid monotony; do they have a favourite glass or mug? Do they like using a straw? Drinking drinks they enjoy and in a familiar glass/mug may lead to an increased intake.
- It makes sense to spread drinks throughout the day to keep vulnerable individuals hydrated and to ensure too much fluid at one time is not making them feel full and interfering with their appetite.
- If anyone has a temperature they should be encouraged to drink more, as they will lose fluid through sweat. If you are concerned about an elderly persons fluid intake, keep a fluid chart and check at the end of the day if they have had enough to drink.
- Offer wet foods – these can add to fluid intake -jelly, ice cream or sorbet, soups, tinned fruit in juice. Several foods have a very high water content i.e. over 84% e.g.melon cucumber, tomatoes, grapes, oranges and apples are good.
- Experiment with drinks at different temperatures.
- Try something new like a smoothie or milkshake.
How hydrated are you?
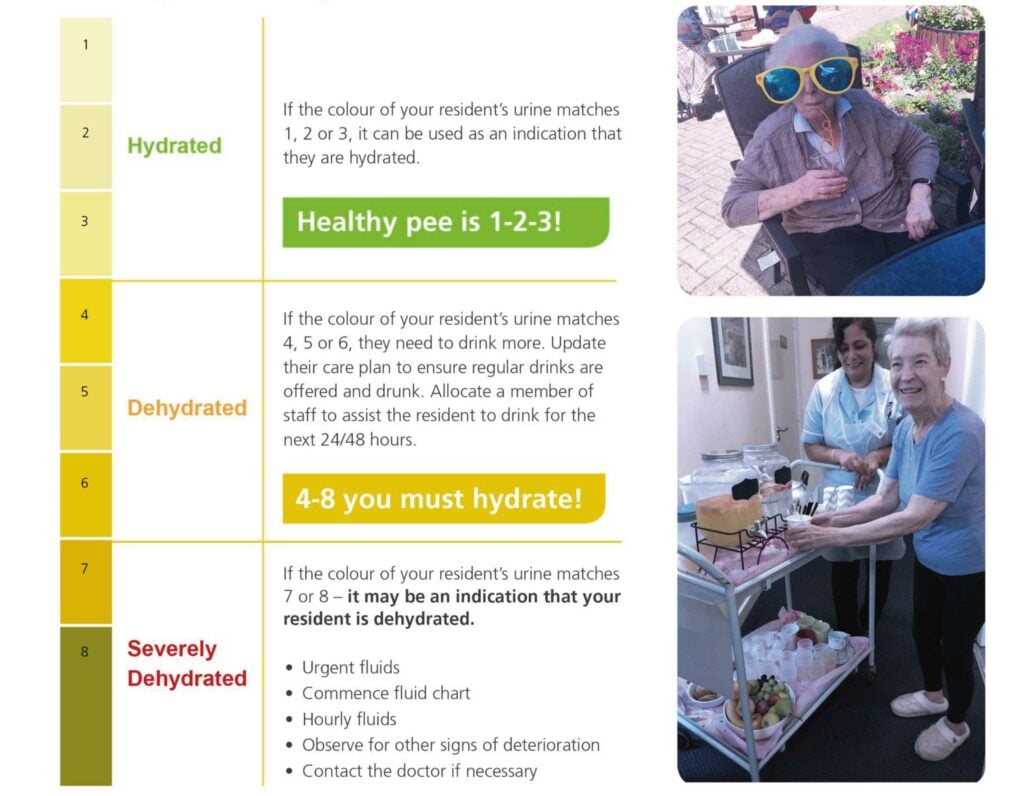
NHS Improvement and the Oxford Patient Safety Collaborative have come up with a useful summary for encouraging good hydration in Care homes. This is useful for any carer or family member looking after an elderly relative.
A good principle of adequate hydration is that the clear and lighter the urine the better
For additional information on a nutrient-rich diet that will help prevent illnesses and injuries see the Eatwell Guide from Public Health England.

